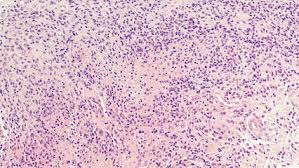
Glioblastoma
Glioblastoma, also termed Glioblastoma Multiforme (GBM), is a malignant fast-growing tumor of the brain or spinal cord. This disease is sometimes referred to as Glioma, as this is the specific cell type that has cancerous proliferation in the disease. There are approximately 200,000 cases in the United States every year, and the current treatment regimens are relatively ineffective. There is no known cure for this tumor, and treatment modalities generally include a combination of chemotherapy, surgery, and/or radiation. There may
also use of OPTUNE therapy along with chemo.
What is Optune® approved to treat? Optune is a wearable, portable, FDA-approved device indicated to treat a type of brain cancer called glioblastoma multiforme (GBM) in adult patients 22 years of age or older
Due to the poor prognosis and low survival rates, new and effective treatments are needed. Research is ongoing and several studies indicate that cannabinoids have been shown to be partly effective in treating the progression of this cancer. For those recently diagnosed and receiving current treatment the average median survival is 15-16 months. This means that half of these patients will survive this time period. Because of the variability in the disease state and treatments, survival rates can be longer but only 5% live for a five-year period after original diagnosis. New therapies are desperately needed to combat this disease and also allow longer survival rates.
The symptoms can be multi-varied and can include headache, nausea, drowsiness, blurred vision, personality changes, seizures, weakness, or facial drooping. Other signs of the disease may also be evident, and a medical diagnosis including imaging with brain MRI and lab tests are required to make a firm diagnosis. This is an emergency situation if the diagnosis is confirmed and requires quick medical attention. Often the tumor is removed or resected, and this can be followed by 7 weeks of radiation and /or chemo, and then possible post-radiation chemotherapy often involving the chemotherapeutic agent Temozolomide (Temodar) or others.
It is well known and accepted that the use of cannabinoids is beneficial to combat the side effects of cancer therapy and help with Quality of Life (QOL) issues such as pain control, anxiety, insomnia, and cachexia (weight loss). This use of cannabis is to mitigate or reduce negative side effects caused by either radiation or chemotherapy, and allows cancer patients to better tolerate their treatment. Cannabis can be especially useful is to treat chemotherapy-induced nausea and vomiting (CINV) and to allow proper rest and rejuvenation that occurs during a normal sleep cycle.
The purpose of this article is to investigate the use of cannabis in Glioblastoma as adjuvant therapy (the use of cannabis in addition to traditional therapy) in order to possibly help combat cancer directly. It is important for patients to receive regular medical care and only use cannabis as a form of supplemental therapy and in conjunction with regular therapy. In general terms, there are many studies showing the benefit of cannabinoids in preventing the growth of tumors and the resultant cell death of cancerous cells (apoptosis – autophagy). Keep in mind that most or all of these studies are done in mice, other animals (in vivo), and still others in test tubes (in vitro). However, there are also some initial studies in humans in a real-life clinical setting using synthetic or phytocannabinoids. Israel and Greece are countries pioneering research in this area, with studies involving glioblastoma patients and various components of cannabis that can be useful during chemotherapy treatments.
It should be noted that researchers are investigating the approximately 140 cannabinoids and their effect on different cancer cell types as far as proliferation, metastasis, and autophagy, and apoptosis (cancer cell death). Groupings of cannabinoids are being investigated and their effect on specific cell types of cancer cells are being studied. It is becoming apparent that each type of cancer cell may require a specific cannabinoid or more likely specific group of cannabinoids, in order to be effective against a particular type of cancer. Some of this ongoing research is being done at Technion Institute in Tel Aviv, Israel by Dr. David Meiri and his lab. Dr. Guzman et. al. are also doing research in Madrid Spain. Some types of cancer cells may be more susceptible to cannabinoids than others, and in some cancer cells, there may be little if any effect. This research will take years to accomplish, and will speed up drastically if the federal restriction of THC is lifted in our country to allow proper research. Groups like the National Cancer Institute (NCI) and National Institutes of Health (NIH) are looking at the research worldwide in this area. The International Cannabinoid Research Society (ICRS) is also currently conducting lab research with mice and cannabinoid synthetic ligands with different groups of cancer cells. More work needs to be done to unlock the possible use of cannabinoids as anti-tumor agents. However, our government health institutions, universities, and scientific research communities are opening up both to accept the research that has already been done and also promote new research in many areas where cannabinoids can be therapeutic.
Glioblastoma therapy usually involves chemotherapy at some point during treatment, and a common agent used is called TEMODAR or temozolomide. Some of the glioblastoma studies focus on this chemotherapeutic agent used in conjunction with either THC or CBD. The goal is to slow or arrest tumor growth, extend survival rates, and kill actual cancer cells more effectively. It has been demonstrated that the standard chemotherapeutic agent Temodar (temozolomide) used in treating this disease, is potentiated and substantially more effective if used in conjunction with several cannabinoids – i.e. THC and CBD. This article will look at some of these studies, the methods used, lab and clinical results, and indications for using THC and CBD in concurrent chemotherapy with Temozolomide for those suffering with Glioblastoma. These cannabinoids may hold other possible benefits in this disease, even when not used with chemotherapy, but in regard to other parameters and mechanisms still being researched. Many studies have shown, at least using mice and synthetic cannabinoids, the benefit to inhibit or slow the growth of many types of cancer cell lines. However, in glioblastoma the standard therapy dictates the benefit of using Temodar, so currently do not use cannabis as a replacement for your chemo, but rather in addition to it.
The studies on Glioblastoma and cannabis started perhaps 20 years ago, and they are still being conducted today. These research studies are being done with the ICRS, Technion Institute, The American Society of Clinical Oncology, GW Pharmaceuticals, American Association of Cancer Research, Molecular Cancer Therapeutics, and many other groups and organizations around the world.
A pioneering study was done by Dr. Manuel Guzman in Madrid in 2011 which is also cited in this article.
One study in the Journal of Clinical Oncology from 2017 was titled “A two-part safety and exploratory efficacy randomized double-blind, placebo-controlled study of a 1:1 ratio of the cannabinoids cannabidiol and delta-9-tetrahydrocannabinol (CBD:THC) plus dose-intense temozolomide in patients with recurrent glioblastoma multiforme (GBM)
This study was done in humans…it was a double-blind randomized placebo-controlled study.
To sum it up, this study came to the conclusion that cannabinoids were sufficiently beneficial if used with chemotherapy in improving survival rates. Compared to a placebo group, those receiving THC and CBD during chemotherapy had a median survival of 550 days as opposed to 369 days without using THC and CBD. One year survival rates were increased from an average of 56% to 83%. Some side effects of therapy were noted but no toxicity.
Another study in Molecular Cancer Therapeutics in 2011 involved glioma xenografts in vitro and found similar results. This is the one done by Dr. Guzman et. al. in Spain.
The abstract of this study showed the following, and much credit should be given to the research group that pioneered this study.
“Glioblastoma multiforme (GBM) is highly resistant to current anticancer treatments, which makes it crucial to find new therapeutic strategies aimed at improving the poor prognosis of patients suffering from this disease. Δ(9)-Tetrahydrocannabinol (THC), the major active ingredient of marijuana, and other cannabinoid receptor agonists inhibit tumor growth in animal models of cancer, including glioma, an effect that relies, at least in part, on the stimulation of autophagy-mediated apoptosis in tumor cells. Here, we show that the combined administration of THC and temozolomide (TMZ; the benchmark agent for the management of GBM) exerts a strong antitumoral action in glioma xenografts, an effect that is also observed in tumors that are resistant to TMZ treatment. Combined administration of THC and TMZ enhanced autophagy, whereas pharmacologic or genetic inhibition of this process prevented TMZ + THC-induced cell death, supporting that activation of autophagy plays a crucial role on the mechanism of action of this drug combination”. Administration of submaximal doses of THC and cannabidiol (CBD; another plant-derived cannabinoid that also induces glioma cell death through a mechanism of action different from that of THC) remarkably reduces the growth of glioma xenografts. Moreover, treatment with TMZ and submaximal doses of THC and CBD produced a strong antitumoral action in both TMZ-sensitive and TMZ-resistant tumors. Altogether, our findings support that the combined administration of TMZ and cannabinoids could be therapeutically exploited for the management of GBM.
These studies, among others, have allowed GW pharmaceuticals to perform phase 2 clinical controlled studies approved by the FDA, as they manufacture a plant-based therapeutic drug called Sativex which may be used in the treatment of GBM. Currently, this drug is allowed in 21 countries but not in the US. However, a similar formulation is available at most US Medical Cannabis dispensaries
Due to the high levels of THC needed in therapy, psychoactivity becomes a limiting factor in most patients being treated and is mitigated by the concurrent use of CBD. This issue of unwanted psychoactivity can also be addressed by ramping up the dose of THC slowly and hopefully building tolerance to allow higher doses. Fortunately, the addition of CBD has been shown to synergize and make the THC more effective than if THC is used alone. Patients should prepare for alteration in lifestyle and perhaps quite a bit of sedation and excessive sleep when using cannabis along with their chemo treatment. Many can cope with the side effects, but some will not. Treatment should last for 6 months on the cannabinoids, and an oral or sublingual dose of strong cannabinoids are needed (i.e. edibles, RSO, Extracts or concentrates). In all honesty, no one really knows the exact specific cannabinoids, dose levels, or administration methods useful in treating this disease optimally. Medical cannabis providers rely on available evidence and research on which cannabinoids to use and how to administer the proper dose. There are no universal guidelines. Specific recommendations and exact dosages for therapies are not generally possible with cannabis at this stage of our knowledge. There are also over 800 compounds in the cannabis plant and each individual may require their own special dosing and strain based on their unique chemistry. Nonetheless, these studies and current research recognizes the benefit of using cannabis with Temodar to increase its effectiveness, prolong survival times, and ease the anguish of this disease. While research results are continually forthcoming, legal challenges and lack of clinical knowledge of cannabinoids may prevent it’s use by all oncologists in our country with this disease. In my opinion, it should be a part of treatment for ALL those who are receiving chemotherapy for GBM, under the guidance of their oncologist.
Dr. Stanley R. Manstof
12201 Greenridge Drive
Boyds, Md. 20841
*MMCC Certified Provider
*American Academy of Cannabis Physicians
*Member Americans for Safe Access
*Technical Writer and Editor
*Member Society of Cannabis Clinicians
*International Cannabinoid Research Society
*Certified Patient Caregiver
301-471-4716 cell
301-972-2700 office
Marylandcannabisconsultants.org
E Mail: drstanman@aol.com